 We are teeming with bacteria, fungi, and viruses. This is a deliberate arrangement that every one of us unwittingly enters into. From the moment we are born, we begin to accumulate and cultivate certain desired microbes. They live without and within, on our skin and in our guts. We co-evolved with the microbes and it’s a mutually beneficial relationship.
We are teeming with bacteria, fungi, and viruses. This is a deliberate arrangement that every one of us unwittingly enters into. From the moment we are born, we begin to accumulate and cultivate certain desired microbes. They live without and within, on our skin and in our guts. We co-evolved with the microbes and it’s a mutually beneficial relationship.
In our intestines, microbes help us with digestion and nutrition. They give us access to the energy stored in some complex carbohydrates that would otherwise just pass through. They make the vitamin K that we need. For that, we give them room and board. It’s a happy relationship.
But these are bacteria, viruses, and fungi. Those are the same words ascribed to infections and disease. How do we make this work?
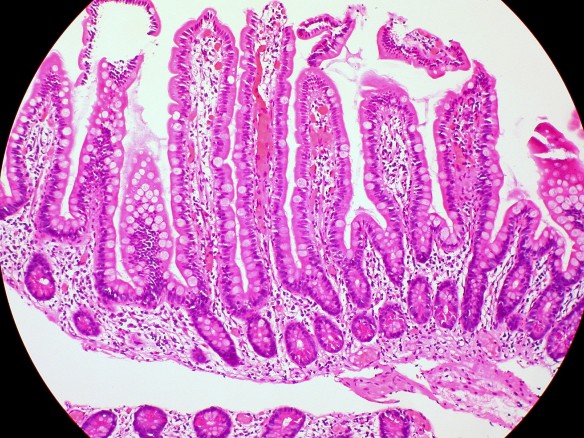
In order to safely contain these microbes, we have constructed barriers and safeguards that separate what’s going on in the gut from the rest of the body. The gut is lined by epithelial tissue with tight junctions between cells to prevent microbes from slipping through. The thick layers of mucous secreted into the intestines are hard for microbes to cross. In that mucous are gut-specific immune cells. They deal with surveying the massive numbers of bacteria within the gut, and reporting back to gut’s immune tissue. Any hardy invaders that bypass these defenses should be picked up by the gut’s lymphatic tissue. Ideally, problems are dealt with before the body’s general immune system has to get involved, which would lead to system-wide infection and inflammation.
The tissue and mucous barriers that restrict microbes to the guts are physical barriers, like walls. In a paper published by David Artis’s group at the University of Pennsylvania in Science on June 8th, 2012, scientists describe the first non-physical barrier known to keep microbes in their place. They found that cells of the immune system secrete a signal that prevents a bacteria called Alcaligenes from being spread throughout the body.
Alcaligenes are relegated to the gut’s immune tissues: Peyer’s Patches and mesenteric lymph nodes, which sit on the other side of that epithelial wall. They sample what sneaks through, keeping a watchful eye out for foreign invaders. So, the same tissues that constantly patrol for invading bacteria have selected one to let in, and they work to keep it there.
In the lab, Alcaligenes are known to secrete antimicrobials that can kill some E. coli, Strep, and Staph. Maybe that’s why the gut has invited these bacteria to call our bodies home. It may be of extra benefit to have them in the Peyer’s Patches, where immune cells sit in wait for foreign invaders. Like a team, the immune cells can detect an invasion, and the Alcaligenes might help eliminate it.
These lymph nodes sit next to the intestines, straddling that physical barrier that our body erected to keep the microbes that help us with digestion from crossing into the rest of the body. So how do we confine the Alcaligenes to those places, if they’re on the other side of the wall?
Innate lymphoid cells, that’s how. Researchers found that innate lymphoid cells secrete a signal, the cytokine IL22, which keeps Alcaligenes in the lymphatic tissue of the gut. When innate lymphoid cells are taken out of the picture, the Alcaligenes disperse throughout the body. Treating mice that are missing innate lymphoid cells with IL22 keeps the Alcaligenes in their place, so it appears to be the secretion of IL22 that contains the Alcaligenes.
If the Alcaligenes escape the gut, the adaptive immune system mounts a response to eliminate them. In the lab, two weeks after Alcaligenes escaped their gut confinement, the only thing remaining were antibodies specific to the bacteria, patrolling for more. But the mice weren’t necessarily good as new. The mice had residual systemic inflammation following the infection.
This research could have bearing on people with chronic or inflammatory diseases. Patients with Crohn’s disease, cancer, HIV, and Hepatitis C infection are more likely to have experienced a system-wide Alcaligenes infection. If we can prevent Alcaligenes from leaving the gut, we may be able to limit inflammation in chronic human diseases, which would improve patient outcome. It’s also another surprising role for innate lymphoid cells, which were only discovered about ten years ago. Scientists are still teasing apart their varied functions. It’s a mixed bag so far. The cells have been implicated as helpful in recovering from the flu and initiating immune responses, to harmful in colitis and asthma. We can add this discovery to the growing list of potential therapeutic targets to treat inflammatory disease.
______________________________
More reading:
There’s a collection of articles on the Science website about the microbiome. And it’s free to anyone in the month of June…a step in the right direction towards open access.
Innate lymphoid cells promote anatomical containment of lymphoid-resident commensal bacteria, Science, vol. 336, 8 June 2012.
Indigenous opportunistic bacteria inhabit mammalian gut-associated lymphoid tissues and share a mucosal antibody-mediated symbiosis, PNAS, vol. 107:16, April 20, 2010.
Crossover immune cells blur the boundaries, Science 8 June 2012: Vol. 336 no. 6086
_______________________________
Photo credit: Thanks to Euthman for the great histology pic on Flickr, kindly available under the Creative Commons license.

Very interesting! Thanks so much for keeping up with the latest research and then “translating” it into common-speak for us non-scientists.
Reblogged this on Science Unraveled and commented:
Super informative post about the microbiome. My two cents is that the number of bacteria within us actually outnumber our own cells. Additionally your microbiome is similar to your fingerprint, its completely unique to you.
Thanks, glad you liked it. Microbiomes are an interesting topic; I’m looking forward to more from this field in the next several years. Scientific American ran a good cover story in its June 2012 issue. Between that and the material on the Science website, I felt like microbiomes were everywhere I turned!